Abstract
Background
The two major types of cold autoimmune hemolytic anemias are cold agglutinin disease (CAD) and paroxysmal cold hemoglobinuria (PCH). In CAD, the cold agglutinin is usually IgM with anti-I specificity. In PCH, the Donath-Landsteiner (DL) antibody is a cold reacting IgG with anti-P specificity. In this study, we describe the clinical and serological characteristics of patients with autoimmune hemolytic anemia positive for both cold agglutinin and DL antibodies.
Methods
On review of our immunohematology reference laboratory database, we identified patients over a 16-year period (January 2000- March 2016) with the following: i) age ≥18 years, ii) hemoglobin (Hb) <12g/dL, iii) positive direct antiglobulin test (DAT) with hemolysis (increased lactate dehydrogenase/low serum haptoglobin/ elevated indirect bilirubin), and iv) tested for both CAD and DL antibodies. We classified the patients into 3 cohorts. Cohort 1 included patients positive for both cold agglutinin (titer ≥1:64) and DL antibodies. Cohort 2 consisted of patients with DL antibody but no cold agglutinin (titer <1:64), while Cohort 3 was comprised of patients with cold agglutinin but no DL antibody. We evaluated the clinical response based on the GIMEMA (Gruppo Italiano Malattie EMatologiche dell'Adulto) criteria (Barcellini W, et al . Blood 2014) defined as i) complete (CR): hemoglobin ≥12 g/dL with normalization of at least one previously abnormal hemolytic marker; ii) partial (PR): hemoglobin 10-12 g/dL with hemolysis; or iii) none (NR): if any of the above criteria were not met.
Results
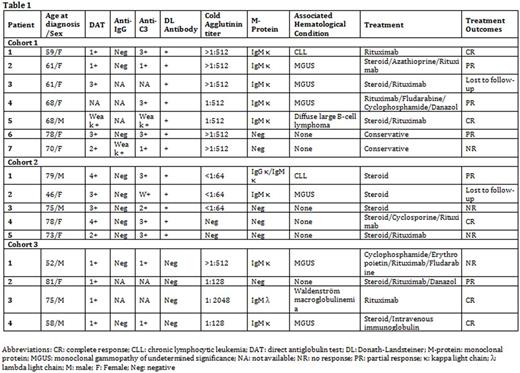
Seven patients had cold autoimmune hemolytic anemia with concomitant cold agglutinin and DL antibodies (Cohort 1). The clinical and serological characteristics are described in table 1. The median age at diagnosis was 68 years (range: 59-78) and the median hemoglobin at onset was 10.3 g/dL (range: 8.2-10.6). Six had red cell agglutination in the blood smear. Two patients had a recent history of infection (1 with Mycoplasma pneumoniae and 1 with upper respiratory tract infection). The median follow-up was 4.8 months (range: 1.0-166.4). Five patients received steroid/other immunosuppressants and two were managed conservatively. The clinical response to treatment was CR in 28.6% patients, PR in 42.9%, and NR in 14.3%. In comparison, Cohort 2 had a 20% CR, 20% PR and 40% NR, while Cohort 3 had a 50% CR, 25% PR and 25% NR, respectively.
Conclusion
Our study is the first series describing patients with cold autoimmune hemolytic anemia with concomitant cold agglutinin and DL antibodies. In terms of clinical response, patients with negative DL antibodies and cold agglutinin titers >1:64 had better response (50% CR, Cohort 3) to immunosuppressants compared to patients with positive DL antibody (20-30% CR, Cohorts 1 and 2). Large scale studies may be warranted to determine the treatment strategies among patients with concomitant DL and high cold agglutinin titers.
Kay: Agios: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Research Funding; Tolero Corporation: Research Funding; Gilead: Research Funding. Winters: Fresenius Kabi USA: Consultancy; Eliaz Therapeutics Inc: Membership on an entity's Board of Directors or advisory committees; Sanofi Inc: Other: Moderated opinion leader's forum; Wiley Blackwell: Employment; Regional Health Inc: Consultancy; Mayo Clinic: Employment; Grifols International SA: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal